Signs Your Back Pain Is Really a Nerve Issue Not Just Muscle Strain

Not all back pain is created equal. While sore, tight muscles are common after a long day or a tough workout, nerve-related pain behaves differently—and recognizing the difference can help you get the right care sooner. If you’re noticing any of the signs below, your pain may involve nerve irritation or compression (often from a disc herniation, spinal stenosis, or inflammation). Here’s what to watch for—and what to do next.
1) Pain that travels or “radiates” down a limb
Muscle pain tends to stay local. Nerve pain often follows a defined path: from your low back into your buttock and down the back or side of your leg (classic sciatica), or from your neck into your shoulder, arm, and hand. That “line” of pain is a hallmark of nerve involvement.
2) Numbness, tingling, or “pins and needles”
These sensations—called paresthesias—suggest altered nerve signaling. You might notice a patchy “asleep” feeling in your thigh, calf, foot, or fingers that comes and goes with certain positions. Muscular soreness rarely causes true numbness.
3) Burning, zapping, or electric-shock pain
Sharp, shooting jolts or a persistent burn often point to irritated nerves. Muscle aches are typically dull, achy, and pressure-like; electricity or fire sensations raise suspicion for nerve compression or inflammation.
4) Weakness in a specific muscle group
Trouble lifting your foot (foot drop), gripping objects, rising onto your toes, or extending your knee can indicate a nerve root isn’t communicating well with its target muscles. This is different from generalized fatigue after exercise; it’s a clear, repeatable strength deficit.
5) Leg pain worse than back pain
When sciatica is present, the leg pain often eclipses the low-back discomfort, especially below the knee. If your “problem area” feels more like your calf or foot than your lumbar muscles, a nerve root may be involved.
6) Coughing, sneezing, or straining spikes the pain
Bearing down (the Valsalva maneuver) increases pressure around the spinal canal. If a cough or sneeze sends a lightning bolt down your leg or arm, it’s a classic sign that a nerve root is sensitive.
7) Changes in reflexes, balance, or coordination
Diminished ankle or knee reflexes, clumsiness with fine motor tasks, or a new tendency to stumble can be subtle but important clues. These neurological signs suggest more than a simple muscle strain.
8) Position-sensitive symptoms (and relief with the opposite)
Nerve pain often flares in specific postures: sitting for long periods, bending forward, or repeated extension. You might also notice the inverse—certain positions (gentle walking, lying on your side with a pillow, or alternating between sitting and standing) reduce the symptoms. That sensitivity to spinal position is common with nerve root irritation.
9) Red-flag nerve symptoms (seek urgent care)
Loss of bowel or bladder control, severe or rapidly worsening weakness, or numbness in the saddle area (inner thighs/groin) requires immediate medical attention. These can indicate a rare but serious condition and should be evaluated in an emergency setting.
What to do next
- Stay gently active. Total bed rest can worsen stiffness and nerve sensitivity. Short walks and frequent position changes (every 20–30 minutes) help circulation and reduce pressure on irritated tissues.
- Use pain-management basics. Heat or ice (whichever feels better), supportive pillows, and over-the-counter analgesics (as advised by a medical professional) can make symptoms more manageable while you seek care.
- Mind your posture. Neutral spine, hips slightly above knees when sitting, feet flat on the floor, and monitor at eye level can reduce nerve tension.
- Know when to get help. Persistent symptoms beyond a couple of weeks, progressive weakness, or any red flags deserve prompt evaluation. Imaging is sometimes helpful, but many nerve-related back issues improve with conservative care.
How conservative care can help
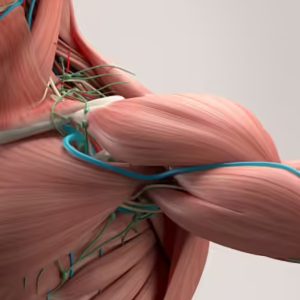
A spine-focused clinician will take a detailed history, perform orthopedic and neurological tests (strength, sensation, reflexes), and determine whether your pain is muscular, joint-related, or nerve-driven. Care plans may include gentle joint mobilization or adjustments, targeted exercises to reduce nerve irritation, soft-tissue work for surrounding tension, and guidance on activity pacing. When appropriate, providers coordinate with primary care or specialists and refer for imaging or advanced care if needed.
If you’re checking several boxes from the list above, consider booking an evaluation with a qualified provider who offers comprehensive chiropractor services to assess nerve involvement and tailor a plan for relief and recovery.
Muscle strains are common—and usually straightforward. Nerve-related back pain has a distinct fingerprint: traveling pain, tingling or numbness, sharp electric sensations, position sensitivity, and specific weakness or reflex changes. Recognizing those signs helps you seek the right care at the right time, get a precise diagnosis, and return to pain-free movement faster.