Peptides in Recovery Science: What Current Research Suggests About Tissue Repair and Performance
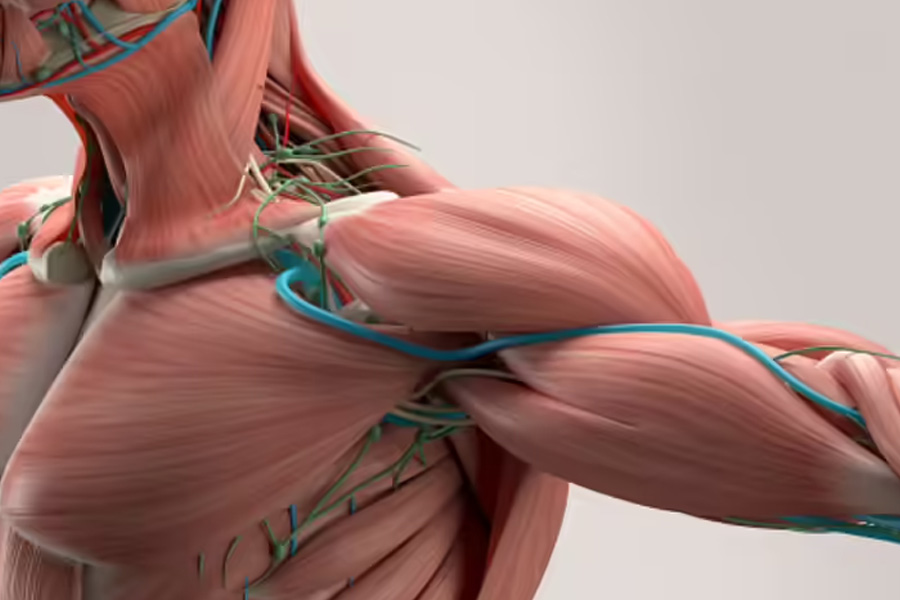
Image Source: health.economictimes.indiatimes.com
Summary
Peptides are gaining attention in research settings for their potential role in tissue repair, inflammation modulation, and recovery signaling. While much of the discussion online is speculative or promotional, this article examines what peptides are, how they function biologically, and what current laboratory research suggests — with an emphasis on regulation, context, and responsible interpretation.
What Are Peptides, Exactly?
Peptides are short chains of amino acids — smaller than full proteins — that function as signaling molecules throughout the body.
Some peptides act as hormones. Others influence immune responses, tissue repair, appetite regulation, or cellular communication. Insulin, for example, is technically a peptide hormone. So are many compounds involved in growth signaling and wound healing.
In research environments, scientists investigate both naturally occurring and synthetic peptides to better understand:
- Tissue regeneration
- Collagen synthesis
- Muscle preservation
- Inflammatory modulation
- Growth factor signaling
The key distinction is that many peptides discussed in performance circles are still under investigation and not approved as therapeutic drugs.
Why Recovery Science Is Paying Attention
Training creates microtrauma. That’s not inherently negative — it’s the stimulus for adaptation.
But the speed and efficiency of repair determine how quickly someone can train productively again.
In laboratory studies, researchers examine peptides that may influence:
- Fibroblast activity
- Angiogenesis (formation of new blood vessels)
- Collagen deposition
- Satellite cell activation in muscle
These mechanisms are complex and highly regulated. Peptides do not “build muscle” in isolation; they interact within intricate biological systems.
The growing interest in recovery optimization has led to more scientific curiosity about signaling pathways — not just mechanical loading.
Collagen, Connective Tissue, and Structural Integrity
Tendons and ligaments adapt more slowly than muscle tissue. This is one reason connective tissue injuries are common in athletes who increase load too quickly.
Collagen synthesis is central to tendon repair. Certain peptides studied in preclinical models appear to influence growth factors associated with connective tissue remodeling.
It is important to emphasize that most of this research remains in early phases. Animal models and in vitro studies often precede robust human trials.
The U.S. Food and Drug Administration has not approved many of the peptides discussed in performance communities for muscle-building or athletic enhancement purposes.
Distinguishing between research exploration and clinical validation is critical.
Inflammation: Suppression vs. Regulation
Inflammation is often portrayed as something to eliminate. In reality, acute inflammation is part of the repair process.
Some peptides under investigation are studied not for eliminating inflammation entirely, but for modulating excessive inflammatory responses. In theory, balanced inflammation may support efficient recovery without prolonging tissue damage.
However, translating laboratory findings into applied human performance outcomes requires caution. Dosing, delivery methods, and long-term safety profiles are still areas of ongoing study.
Muscle Signaling and Growth Factors
Muscle adaptation is governed by pathways such as mTOR activation, IGF-1 signaling, and satellite cell proliferation.
In research environments, certain peptides are examined for how they interact with these pathways. The goal is often to better understand muscle-wasting conditions or injury recovery — not to enhance athletic performance.
Regulatory bodies such as the World Anti-Doping Agency prohibit many growth-factor-related compounds in competitive sport.
That regulatory context matters. Scientific exploration does not equal general use approval.
The Importance of Evidence Hierarchy
When evaluating peptides — or any emerging compound — understanding levels of evidence is essential:
1. In vitro (cell culture) studies
2. Animal models
3. Early-phase human trials
4. Large-scale randomized controlled trials
5. Long-term safety monitoring
Much of what circulates online stops at levels one or two.
For readers who want a structured breakdown of mechanisms, regulatory status, and summaries of published data without exaggerated claims, this independent educational peptide research guide compiles findings from available literature in a neutral format:
A comprehensive review of current peptide research and mechanistic studies
Approaching the topic with context allows informed discussion without overstatement.
Sleep, Nutrition, and Peptide Signaling
Before exploring experimental recovery tools, foundational variables deserve attention.
Sleep directly influences growth hormone pulses.
Protein intake supports amino acid availability.
Resistance training stimulates natural anabolic signaling.
Adequate caloric intake prevents catabolic stress.
The National Sleep Foundation emphasizes sleep duration and quality as core determinants of physical restoration.
In many cases, optimizing these variables produces measurable improvements in recovery capacity without introducing experimental compounds.
Emerging research does not replace fundamentals — it builds upon them.
Risk, Regulation, and Responsible Framing
A recurring issue in online discussions is the leap from “being studied” to “proven effective.”
Many peptides:
- Lack long-term human safety data
- Are not approved medications
- Are restricted in sport
- May be misrepresented in marketing contexts
Responsible conversation requires separating laboratory curiosity from clinical consensus.
Scientists study mechanisms to understand biology. That doesn’t automatically translate into broad application.
Practical Recovery Strategies That Remain Foundational
While research into signaling molecules continues, the strongest evidence for recovery still supports:
- Progressive resistance training
- Structured deload phases
- Sufficient protein distribution
- Electrolyte-balanced hydration
- Consistent sleep schedules
- Stress management
These variables directly influence the same pathways that peptides aim to modulate.
In other words, biology already contains powerful systems for repair. Lifestyle and training choices determine how effectively they function.
The Bigger Picture
Peptides represent a fascinating area of scientific exploration. Understanding how small amino acid chains influence cellular signaling expands our knowledge of tissue repair, inflammation, and muscle biology.
But the conversation must remain grounded.
Performance enhancement claims often outpace evidence. Regulatory status matters. Long-term human data matters even more.
For readers interested in exploring the science itself — not hype — reviewing structured summaries of published peptide research can provide valuable context. Mechanisms are complex, and interpretation requires nuance.
Recovery is multifactorial. No single compound replaces intelligent programming, adequate nutrition, and restorative sleep.
Conclusion
The growing interest in peptides reflects a broader trend in performance culture: a desire to understand recovery at the molecular level.
That curiosity is not inherently misguided. Science advances through exploration.
However, adaptation remains rooted in fundamentals:
- Mechanical tension
- Metabolic stress
- Restorative sleep
- Nutritional sufficiency
- Nervous system regulation
Peptides are being studied within this broader biological framework — not outside of it.
As research evolves, responsible interpretation will remain essential. Education, context, and evidence hierarchy should guide the discussion.
Because in performance — as in health — sustainability always outweighs shortcuts.